The Benefits of Rehabilitation
The Role of Rehabilitation
 Rehabilitation can be of significant benefit to an individual who is experiencing a change in his or her physical abilities. Most people are familiar with the importance of rehabilitation following surgery, injury, or stroke. More recently, the medical community has come to recognize the enormous value of ongoing rehabilitation for people with chronic illness, particularly MS, whose variety of changing symptoms can affect virtually all areas of movement and function.
Rehabilitation can be of significant benefit to an individual who is experiencing a change in his or her physical abilities. Most people are familiar with the importance of rehabilitation following surgery, injury, or stroke. More recently, the medical community has come to recognize the enormous value of ongoing rehabilitation for people with chronic illness, particularly MS, whose variety of changing symptoms can affect virtually all areas of movement and function.
Rehabilitation addresses many of the issues and challenges experienced by individuals with MS. Some of the specific symptoms that may be helped include spasticity, weakness, and resultant movement problems; balance, dizziness, and coordination difficulties; as well as changes in speech, swallowing, cognition, and vision. Treating these specific symptoms, however, is only the beginning. Limitations in movement and other abilities affect many other aspects of everyday life, and the different types of therapy offered through rehabilitation work to regain, or find ways to compensate for, lost function. Safety precautions and the prevention of pressure sores are also vital issues that are promoted through rehabilitation.
MS symptoms impact how someone is able to function at work and at home. They affect one’s ability to drive or participate in outside activities. They also play a big role in one’s self image and how an individual interacts with others. As a result, social, psychological, and emotional changes coincide with the onset of physical symptoms.
The unique and wonderful concept behind rehabilitation is that it incorporates an individual’s entire situation, taking into account how physical changes may impact one’s activities, emotions, and well-being. With rehabilitation, a team of specialists work together to address all aspects of an individual’s disability. Their overall goal is to improve a person’s quality of life, while helping preserve one’s independence and safety.
Rehabilitation Terms, Facilities, and Insurance Coverage
Following an exacerbation or flare-up of symptoms, individuals are often referred to rehabilitation to help regain lost function. This is an opportunity to gradually get the muscles moving again and to begin an exercise program that will help the individual return to his or her normal lifestyle and activities as soon as possible. Attention is given to any symptoms which did not subside, and various therapies and/or assistive devices are recommended to help the individual cope with these changes. When necessary, the participant learns “compensatory techniques,” enabling him or her to accomplish tasks in different ways than before, to substitute for any lost ability.
 Rehabilitation is also extremely beneficial to individuals who are not having a flare-up but who are experiencing symptoms. Physical therapy, occupational therapy, speech therapy, and recreational therapy can all help to relieve certain symptoms, increase function, and provide an emotional boost for someone with MS.
Rehabilitation is also extremely beneficial to individuals who are not having a flare-up but who are experiencing symptoms. Physical therapy, occupational therapy, speech therapy, and recreational therapy can all help to relieve certain symptoms, increase function, and provide an emotional boost for someone with MS.
Initial rehabilitation is referred to as “restorative,” because it is aimed at bringing an individual to his or her highest functioning potential. Specific goals are set and insurance commonly covers this type of rehabilitation. After a person has reached his or her full potential for improvement, treatment is then referred to as “maintenance” rehabilitation, which is aimed at preventing any decrease in function. While this latter type of therapy is extremely important for keeping someone on track, insurance companies are not as quick to pay for maintenance rehabilitation.
“Preventative” rehabilitation is the new term for maintaining function, and because specific goals are set, this is viewed as a more dynamic process, encouraging insurance companies to approve funding.
If inpatient rehabilitation is prescribed by a physician, the individual will stay at an acute or subacute rehabilitation facility. In contrast to acute care, a subacute facility is less aggressive and less expensive. Often associated with the acute care facility, subacute care is a good intermediate treatment that helps make the transition between the hospital and returning home easier. Daily sessions with subacute care are typically three hours in length. On average, Medicare will pay for two to three weeks of therapy, while other insurance may pay for a seven to 10-day stay.
Outpatient rehabilitation offers several advantages and is growing in popularity. It enables clients to experience the benefits of rehabilitation without having to stay for a week or more away from home. Outpatient rehabilitation centers provide much of the same equipment and personnel found at the larger acute and subacute care facilities, but they may be located closer to a patient’s home. They may also be smaller, more personal, and lower-key, so the participant may feel more comfortable. These types of facilities serve to reinforce and further progress skills learned earlier in the inpatient setting.
Individuals who attend an outpatient facility often have sessions two to three days per week.
Outpatient centers are much less expensive than acute and subacute care, with insurance usually covering a certain number of visits per year. Different therapies (discussed later) are provided, typically requiring one hour per visit for each. An outpatient rehab facility will try to schedule different therapy sessions at consecutive times on the same day, so the client does not need to make separate trips when seeing more than one therapist.
Clients need to be aware, however, that each one-hour appointment with a therapist is considered by insurance companies to be separate visits – so seeing three therapists for three days at a center could quickly use up nine allowed visits. Before beginning therapy, a representative at the center will need to find out how many visits are covered by insurance, and work with the therapists to design an optimal plan. When the number of visits has reached the limit, members of the healthcare team may try to get additional visits approved.
Clients may also act as their own advocate to request additional coverage from their insurance company. When other options have been exhausted, people seeking a continuation of their therapy should talk directly to someone at their facility. Many outpatient centers offer reduced rates and payment plans so that individuals who have run out of insurance coverage may continue with therapy.
 Therapists occasionally provide home visits. This may be an option for an individual who has difficulty traveling or who lives too far from an outpatient rehab facility. While this adds convenience for the client and can provide much-needed therapy, the disadvantages of this include not having access to all the equipment and personnel at the facility, as well as missing out on the social aspect of going out to a center. Therapists may also visit a home or workplace to recommend strategies and assistive equipment which will make an environment safer, more comfortable, easier to work in, and more conducive to conserving energy.
Therapists occasionally provide home visits. This may be an option for an individual who has difficulty traveling or who lives too far from an outpatient rehab facility. While this adds convenience for the client and can provide much-needed therapy, the disadvantages of this include not having access to all the equipment and personnel at the facility, as well as missing out on the social aspect of going out to a center. Therapists may also visit a home or workplace to recommend strategies and assistive equipment which will make an environment safer, more comfortable, easier to work in, and more conducive to conserving energy.
According to Linda A. Lucuski, MPT, rehab center administrator and physical therapist, “There are various steps one must take before their first evaluation at a comprehensive rehab center. Although most states do not require a prescription or referral for therapy, most insurance companies will not pay for therapy unless prescribed by a physician. A primary care physician, neurologist, or other licensed physician may write a prescription. The physician and therapist may determine together the frequency and duration of the therapy sessions and the goals to be met.
“When seeking therapy, a representative of the chosen therapy center should be contacted to make sure that the facility participates with the patient’s medical insurance company. Co-pays, deductibles, or co-insurances may be required depending on the insurance company and the plan benefits. In addition to checking for insurance participation, an individual needs to confirm that the center specializes in therapy for individuals with MS. Some rehab centers focus on sports injuries and may not be appropriate for someone dealing with changes caused by MS. If possible, an individual, family member, and/or care partner may tour a facility in advance to see if it has a positive and motivational atmosphere, along with reconfirming that the center has experience treating MS.”
How Rehabilitation and Exercise Help People with MS
Rehabilitation is often prescribed after an exacerbation subsides. This may help regain lost function as well as gradually return someone to his or her previous level of activity. When one’s MS is stable, rehabilitation may still be recommended. Whether a person has mild, moderate, or more advanced MS, he or she may derive much benefit from one or more types of therapy.
 With mild MS, a participant may learn about the disorder, managing symptoms, proper exercise, dietary recommendations, and general health. With moderate MS, more aggressive therapy is needed, often assisting with activities of daily living (ADL); ambulatory aids (such as a cane or walker); exercises for mobility, balance, and coordination; assistive devices (such as a hand or leg brace); and possibly speech or cognition exercises. With more advanced MS, other adaptive equipment may be recommended, and much attention is given to time spent in a wheelchair. In addition to exercise and safety issues, customizing the fit of the wheelchair and avoiding further complications such as pressure sores are emphasized.
With mild MS, a participant may learn about the disorder, managing symptoms, proper exercise, dietary recommendations, and general health. With moderate MS, more aggressive therapy is needed, often assisting with activities of daily living (ADL); ambulatory aids (such as a cane or walker); exercises for mobility, balance, and coordination; assistive devices (such as a hand or leg brace); and possibly speech or cognition exercises. With more advanced MS, other adaptive equipment may be recommended, and much attention is given to time spent in a wheelchair. In addition to exercise and safety issues, customizing the fit of the wheelchair and avoiding further complications such as pressure sores are emphasized.
Rehabilitation can often help symptoms such as spasticity or weakness, which can create an imbalance. This can cause an individual to overuse certain muscles while other muscles weaken because of disuse. Even someone with very few symptoms may not realize that his or her gait has changed and is not moving as smoothly as one should. Numbness, pain, or changes in sensation can also lead to problems with walking and other movement, including overextension of the knee.
Dizziness, balance, and coordination problems may all be helped through “vestibular” rehabilitation. “Proprioception” is the ability to detect what position a joint or limb is in at any given time (allowing someone to know where limbs, hands, and feet are when a person’s eyes are closed). Therapists work to improve individuals’ awareness of where their hands or feet may be through exercises that help with sensory input. Tremor may be lessened through various techniques such as using a splint or adding weights. Some facilities may also offer therapy for individuals with visual changes.
If an individual is having problems doing everyday household chores, rehabilitation can work to teach this person how to accomplish the same tasks in different and safer ways, sometimes with the use of a brace or other assistive device. The same is true for dressing, bathing, and grooming. Rehabilitation facilities are set up to help and instruct individuals to learn new methods for doing “activities of daily living” (ADL), and energy-saving techniques are emphasized to help avoid fatigue.
Individuals with MS may also be helped through rehabilitation by becoming more fit and having an exercise plan. A person who is not exercising will “decondition,” a syndrome which reduces muscular strength, vital capacity (volume of exhaled air), and adrenocortical reserve (stored hormone needed for stress reactions). Deconditioning also increases neuromuscular tension, resting pulse rate, fatigue, anxiety, and depression.
The benefits of aerobic exercise include increased lean muscle mass, flexibility, and tone, while decreasing body fat. It improves heart and lung function, along with positive changes to the blood. Aerobic exercise also decreases anxiety, depression, and fatigue. It raises self-esteem, helps people to sleep better, and improves one’s ability to concentrate and perform better academically.
When doing any exercise routine, participants should always warm up to start and cool down when finished. Exercising three to four times per week is considered to be an optimal amount. Family members may also take part in exercise, allowing everyone to participate for better health.
Anyone planning to initiate an exercise program or make a change in his or her present level of activity should always do so under the guidance of a qualified physician. Particularly with MS, physical activity needs to be started slowly, increased gradually, and carefully monitored by a professional.
When working with people who have MS, therapists need to keep certain limitations in mind. For instance, individuals with MS can become fatigued or overheated quickly. The temperature and time of day can greatly affect someone’s ability to perform. When working out with exercise machines or weights, increases are usually based on repetitions versus increasing weight, which helps to avoid fatigue.
While many symptoms of MS may be better managed through rehabilitation, participating in such a program has another significant advantage. Frequently individuals with MS who undergo physical and other types of therapy at a rehabilitation center find that the experience greatly lifts their spirits.
Exercise can make people feel better physically and mentally, and being in a setting where others have similar or more severe conditions, and to see them getting the benefit of exercise, can help one feel better about his or her self. Additionally, as individuals learn new ways to perform ADL, such as housework, bathing, and other day-to-day activities, they can become more independent, which increases their level of confidence and feelings of self-worth.
Members of the Rehabilitation Team
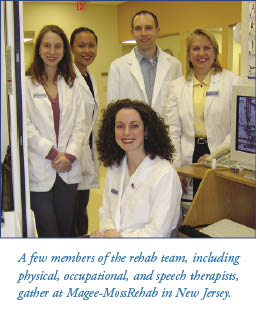 Rehabilitation uses a team approach to address the many issues that MS presents. Several medical professionals may be involved with the therapy that one patient receives. This is an “interdisciplinary” team approach – one in which all members with different specialties work together and discuss a person’s treatment, in contrast to a “multidisciplinary” team, which includes several different specialists who work
Rehabilitation uses a team approach to address the many issues that MS presents. Several medical professionals may be involved with the therapy that one patient receives. This is an “interdisciplinary” team approach – one in which all members with different specialties work together and discuss a person’s treatment, in contrast to a “multidisciplinary” team, which includes several different specialists who work
independently while treating the same individual.
When someone goes to a rehab center for the first time, he or she meets with the different therapists and other professionals who will be working with him or her. From there, specialists meet with the client individually and perform various tests to make an initial assessment. This will provide a baseline measurement of function, from which goals may be set and progress may be determined.
After a thorough evaluation has been completed, the rehabilitation team meets to decide on attainable goals to set for the client in several areas of functioning. A plan is developed to meet these goals, and the team meets with the client, family members, and/or care partner to discuss the overall plan.
Team members who work at a rehabilitation facility may include:
Nurse – The rehab nurse acts as a patient advocate, helping the client and family to understand their choices, develop problem-solving strategies, and set goals. He or she may also perform physical care, assist with evaluation, and oversee coordination of therapies.
Physical therapist (PT) – The role of the PT is to assist individuals in reaching their maximum potential in terms of function, strength, and mobility. The PT is primarily involved with posture, movement, and the lower extremities, giving special attention to safety and energy conservation. This specialist also handles assistive equipment, including the selection and fit of a wheelchair.
Occupational therapist (OT) – The OT focuses on how someone is “occupied” in life, and how they go about ADL (activities of daily living). This specialist works largely with the upper extremities and fine-motor control, but also assesses cognitive status and assists with fatigue management, energy conservation, and safety.
Speech-language pathologist (SLP) or speech therapist (ST) – A speech specialist addresses speech, communication, and swallowing disorders. The SLP also treats cognitive issues, which may be involved. Much work is done with therapy that may include computers and assistive technology to help someone function to his or her full potential.
Recreational therapist (RT) – Using recreation as a tool for improving one’s physical, emotional, and/or social behavior, an RT works with a client’s skills and interests to develop a plan for helping him or her through leisure activities.
Social worker – This person looks at a client’s total living situation, including family dynamics and home environment. A social worker may serve as the case manager and counselor, along with helping to set up any financial arrangements that need to be made for rehabilitation.
Other team members may include: a physiatrist (trained to assess functional issues and the management of symptoms; may act as team leader); a psychologist (to support, counsel, and prepare client and family for active participation in rehab); and a vocational rehab counselor (works with the client to set realistic goals and develop strategies to assist an individual in the workplace or other vocation).
As dictated by an individual’s specific symptoms, additional professionals may be involved with the treatment process. These may include an orthotist, neurologist, respiratory therapist, urologist, chaplain, ophthalmologist, driver education specialist, dietician, and medical equipment vendors.
Different Types of Therapy, Exercise, and Equipment
Physical Therapy
 Physical therapy may be the first thing that comes to mind when thinking of rehabilitation. It covers an enormous range of functions and ability levels, from a slight gait problem to exercises for someone using a wheelchair. This may be the largest area of a rehab facility, packed with a variety of exercise equipment for increasing strength, tone, flexibility, and conditioning, as well as many special products and equipment to help with retraining someone to have better balance and control. As mentioned earlier, the physical therapist (PT) is primarily involved with posture, movement, and the lower extremities, giving special attention to safety and energy conservation.
Physical therapy may be the first thing that comes to mind when thinking of rehabilitation. It covers an enormous range of functions and ability levels, from a slight gait problem to exercises for someone using a wheelchair. This may be the largest area of a rehab facility, packed with a variety of exercise equipment for increasing strength, tone, flexibility, and conditioning, as well as many special products and equipment to help with retraining someone to have better balance and control. As mentioned earlier, the physical therapist (PT) is primarily involved with posture, movement, and the lower extremities, giving special attention to safety and energy conservation.
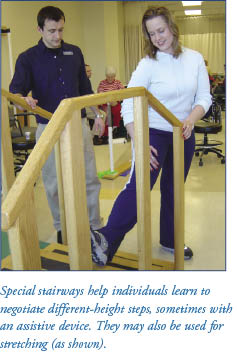
Spasticity is a common symptom of MS and stretching exercises can be very beneficial as a treatment. These should be performed once daily and a printout of a client’s exercise plan and daily “homework” is sent home with the participant. The therapist will repeat movement patterns to correct abnormal posture, which may also inhibit spasticity and spasms.
 Many tools are used to help reduce problems associated with dizziness, balance, and coordination. In general, the therapist must work gradually with the client, starting from a low center of gravity and moving up a high center of gravity. The same is true for a support base, progressing from wide to narrow.
Many tools are used to help reduce problems associated with dizziness, balance, and coordination. In general, the therapist must work gradually with the client, starting from a low center of gravity and moving up a high center of gravity. The same is true for a support base, progressing from wide to narrow.
Giant physioballs (originally from Europe) can help someone to develop better balance as he or she sits on the ball and leans in different directions. A tilt board is also used to help develop better balance. This is a flat piece of wood with a curved piece underneath, causing it to tip from side to side when someone stands on it.
Sometimes small orange cones are placed in a pattern and the participant must maneuver around the cones. This simulates having to walk around various objects at a store or people in a crowd. While holding a belt around the participant’s waist, the therapist may lightly push or bump into the person, helping him or her learn to recover balance when maneuvering in a crowded place.
 Wooden steps set at different heights are used to help individuals practice to safely go up and down different stairways or curbs. A separate step simulates the height of a step getting onto a bus, and this is used for those who take public transportation. If any type of assistive equipment is needed (such as a cane, crutch, or walker), the therapist teaches the individual how to negotiate steps with the device.
Wooden steps set at different heights are used to help individuals practice to safely go up and down different stairways or curbs. A separate step simulates the height of a step getting onto a bus, and this is used for those who take public transportation. If any type of assistive equipment is needed (such as a cane, crutch, or walker), the therapist teaches the individual how to negotiate steps with the device.
A laptop computer connected with two “foot plates” measures how evenly an individual distributes his or her weight. This can be used with hands as well, and indicates if a person is favoring one side over another, helping the therapist to see what side may be more affected.
Some facilities may have low mats on wooden frames that are at the height of a bed. These are used for exercise and to practice getting in and out of a bed, or transferring to and from a chair. Treatment tables may also be found in this area, and this is where a client may receive massage or therapeutic modalities such as light therapy, electrical stimulation, or ultrasound.
Parallel bars are used for individuals who are working to regain the strength and balance needed to walk. They may also be used to practice lifting oneself in and out of a wheelchair.
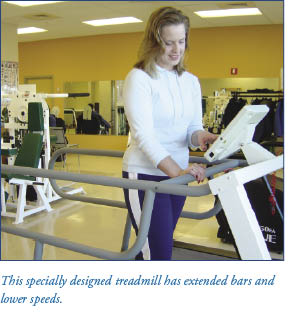
 The physical therapy area has several pieces of equipment for increasing strength and conditioning. Examples include treadmills, stationary bikes, rowing machines, and stair climbers. Many of these have special features for therapy. For instance, a treadmill may have longer bars along the sides and slower speeds; bikes have both foot pedals as well as hand pedals; and a special boot that attaches to the bike is available for individuals experiencing weakness in a leg. Elastic bands called “Therabands®” help with shoulder range of motion, while also serving to strengthen weak muscles and stretch tight muscles.
The physical therapy area has several pieces of equipment for increasing strength and conditioning. Examples include treadmills, stationary bikes, rowing machines, and stair climbers. Many of these have special features for therapy. For instance, a treadmill may have longer bars along the sides and slower speeds; bikes have both foot pedals as well as hand pedals; and a special boot that attaches to the bike is available for individuals experiencing weakness in a leg. Elastic bands called “Therabands®” help with shoulder range of motion, while also serving to strengthen weak muscles and stretch tight muscles.
Individuals not under the guidance of a PT should be cautioned about overuse of exercise equipment. Often a person who is returning to exercise wants to immediately go back to the previous level of exercise (before developing symptoms of MS) and this can cause overexertion and fatigued muscles. A PT will make a schedule that allows the participant to gradually increase their activity level without causing any harm or discomfort.
 If any type of ambulatory aid is needed, such as a cane, crutches, or a walker, the physical therapist makes sure that the correct device is selected, fits properly, and is used correctly. Anyone in need of an assistive device should always see a PT for optimal results and to avoid further injury. A PT also makes custom braces for the lower extremities, including an ankle-foot orthoses (AFO) which can help with symptoms such as foot drop, toe drag, poor knee control, weakness, spasticity, and issues with gait, proprioception, and sensory problems.
If any type of ambulatory aid is needed, such as a cane, crutches, or a walker, the physical therapist makes sure that the correct device is selected, fits properly, and is used correctly. Anyone in need of an assistive device should always see a PT for optimal results and to avoid further injury. A PT also makes custom braces for the lower extremities, including an ankle-foot orthoses (AFO) which can help with symptoms such as foot drop, toe drag, poor knee control, weakness, spasticity, and issues with gait, proprioception, and sensory problems.
A PT also works closely with individuals in wheelchairs. The selection and fitting of a wheelchair is both an art and a science, and many things including a person’s size, posture, strength, and symptoms must be considered. Several types of cushions, wedges, pads, and supports (all of which may be filled with air, foam, or gel) and contoured seating systems are used to ensure maximum comfort and protection from pressure sores.
Prevention of skin breakdown is critical and patients are divided into three categories: low (able to transfer without assistance and shift weight easily), medium (can do pressure relief exercises), and high-risk (needs assistance to perform pressure relief exercises). Different pressure relief maneuvers are taught to the individual and his or her care partner. Among others, these may include lifting up periodically from the chair, leaning from one side to another, and tilting the wheelchair.
Physical Therapist Linda Lucuski points out, “A physical therapist will evaluate an individual’s posture, range of motion of all extremities and the trunk; as well as assess strength, proprioception, balance, coordination and function. The therapist will also assess gait, the ability to walk with or without an assistive device, or evaluate an individual’s wheelchair for proper fit, comfort, and ease of use. The individual’s goals are discussed, and upon completion of the evaluation, a treatment plan will be formulated.
“Follow-up treatment sessions will be scheduled, taking into account the individual’s most productive time of the day and his or her transportation requirements. Treatment sessions will consist of individualized exercises and activities to meet the stated goals. Specialized treatment plans are available for people with neck or back pain, loss of joint mobility of the extremities, as well as balance and coordination problems.”
Occupational Therapy
The occupational therapist (OT) is concerned with how individuals occupy their time and how they function in their ADL (activities of daily living). The OT mostly works with upper extremities, fine-motor skills, and eye-hand coordination.
 For developing strength, several types of hand-strengthening devices are available for grasping and squeezing. Putty is used for rolling, gripping, and to practice cutting.
For developing strength, several types of hand-strengthening devices are available for grasping and squeezing. Putty is used for rolling, gripping, and to practice cutting.
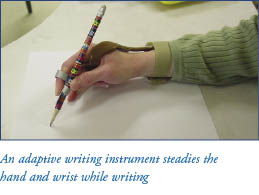
A variety of peg boards, in different sizes and levels of complexity, help individuals to regain coordination. The OT can create finger and hand support if needed for writing (due to weakness or tremor), or a splint to support a contracture. An OT also makes arm braces for those requiring added support. Other devices are available to assist with using a computer keyboard.
The occupational therapy area of a rehab facility is particularly interesting. It may include working kitchens, laundry rooms, and bathrooms – just like someone’s home – to learn and practice techniques for accomplishing everyday tasks. The therapist works with individuals to practice regular household chores such as washing dishes; washing, drying, and folding laundry; and preparing a meal. Additionally, bathrooms are set up with special toilet seats, grab rails, tub seats, and roll-in showers to help individuals learn how to transfer from one seat to another.
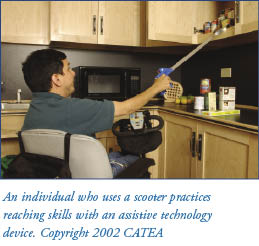 Throughout the different areas, an OT will teach individuals techniques that will help conserve energy and promote safety. Assistive devices are often used as well, and these include long-handled sponges for washing; dressing aids that can help with buttons, zippers, socks, and shoes; and specially designed plates, cups, and utensils.
Throughout the different areas, an OT will teach individuals techniques that will help conserve energy and promote safety. Assistive devices are often used as well, and these include long-handled sponges for washing; dressing aids that can help with buttons, zippers, socks, and shoes; and specially designed plates, cups, and utensils.
The OT may also be involved with workplace intervention. This can include visiting a person’s office or work environment to evaluate safety, comfort, and efficiency. An OT will make recommendations for improving these issues, such as rearranging furniture, relocating someone’s office closer to the exit and restrooms, and adding various types of adaptive equipment. Other suggestions may be made to help with symptoms of MS, and these may include a flexible work schedule, a longer lunch break to allow for rest, and making sure the office is kept at a comfortable temperature.
 Linda Lucuski explains, “An occupational therapist will evaluate an individual with MS for range of motion, strength, sensation, and tone of the upper extremities. The occupational therapist will also evaluate functional activities such as feeding, dressing, bathing, and other activities of daily living. The individual’s physical
Linda Lucuski explains, “An occupational therapist will evaluate an individual with MS for range of motion, strength, sensation, and tone of the upper extremities. The occupational therapist will also evaluate functional activities such as feeding, dressing, bathing, and other activities of daily living. The individual’s physical
environment at home or work may be evaluated and discussed as well.”
“The therapist will then suggest appropriate adaptations as needed to allow ease of movement and function. An example would be an adaptive writing instrument to steady the hand and wrist during handwriting activities such as paying bills and check writing. The occupational therapist will evaluate the upper extremity for any contracture and may fabricate a splint to reduce the contracture, provide joint protection, or to facilitate better movement and function of the hand, wrist or arm.”
Functional Vision Rehabilitation
A specialty program within the field of occupational therapy is the Functional Vision Rehabilitation program. This program, as prescribed by an optometrist, ophthalmologist, neurologist, or primary care physician, is designed to help with visual dysfunction symptoms common in people with MS. These may include blurred or double vision, loss of visual field, and loss of function due to low vision. This type of therapy is only offered at a limited number of centers across the country, but can be very helpful for those fortunate enough to have access to this program.
The therapist may offer recommendations and compensatory techniques to improve the ability of the eyes to function during work, home, and leisure activities. An example would be to use contrasting colors around the home to increase visibility. Low-vision aids are also available, including a device that identifies a medication by its size and color – so someone who is visually impaired may be sure he or she is taking the right prescription at the right time.
Speech Therapy
Voice and articulation problems can be a symptom of MS. This problem may be due to dysarthria, defined as a disorder of movement due to abnormal muscle use which may affect the strength, range, timing, or accuracy of speech movements.
A speech-language pathologist (SLP) is a therapist with training in the evaluation and treatment of speech, language, swallowing, and cognitive problems. The SLP may perform a thorough oral-motor exam to assess the strength, range of motion, speed, timing, and accuracy of the mouth, jaw, and surrounding muscles. The therapist will assess the intensity, speed, coordination, and endurance of an individual’s voice use. Assessment of respiration and proper use of breath is also performed.
Following completion of the evaluation, the SLP will design a comprehensive rehabilitation program which may include oral motor exercises to maintain muscle coordination and strength; pacing or pausing techniques for people whose speech has become slurred and/or rapid. In severe cases of speech problems, nonverbal techniques using a communication board or computer system may be taught.
Individuals with MS may also experience dysphagia, or difficulty swallowing. Dysphagia is diagnosed by an examination of the tongue and swallowing muscles as well as an observation of swallowing different foods and liquids. The therapist may recommend an assistive device (such as a special cup), dietary changes, and exercises to improve swallowing.
Individuals with MS may experience cognitive changes. Cognition is an individual’s capacity to process and use what is heard, touched, seen, smelled, and tasted. Other components of cognition that may be affected are attention, learning and remembering, organizing, comprehension, reasoning, and problem solving. Stress, anxiety, fatigue, and depression may also impact cognition.
The SLP may offer methods to restore cognitive functioning and teach techniques to modify the problem. Cognitive devices or aids such as voice recorders or calendar planners may be introduced. Workbooks and special computer software may also be used in the treatment of cognitive changes.
Recreational Therapy
This form of therapy uses different types of leisure activities to encourage positive physical, emotional, and social changes. Examples include swimming, yoga, and hippotherapy (horseback riding). All of these activities promote physical fitness, involve the participants in an enjoyable activity, and exposes them to other individuals, providing social benefits.
At some rehab facilities, including the Magee-MossRehab center, a golf rehab program is offered for the golfer with difficulties due to symptoms associated with MS.
In Conclusion
 Although many types of therapies and activities are mentioned in this article, space does not allow for a full description of all rehabilitation programs. Hopefully those reading this article will get a better idea of what takes place at a rehab facility and how individuals may be helped with everyday activities and symptom management.
Although many types of therapies and activities are mentioned in this article, space does not allow for a full description of all rehabilitation programs. Hopefully those reading this article will get a better idea of what takes place at a rehab facility and how individuals may be helped with everyday activities and symptom management.
Linda Lucuski concludes, “An individual with MS will benefit most from a therapist who has experience with the evaluation and treatment of dysfunction due to MS. The therapist should spend one-on-one time with the individual, provide encouragement, and take an active interest in the patient’s rehabilitation goals. The right team can make all the difference in the world.”
Anyone who is experiencing symptoms and has yet to receive therapy, or who has not attended recently, may want to discuss the advantages of rehabilitation with his or her healthcare professional. For more information about rehabilitation and MS, please contact MSAA’s Helpline at (800) 532-7667. Individuals may also refer to one of the following contacts. Books on the topic may be found in MSAA’s lending library; please see p. 48 for more information.
Special thanks go to Linda A. Lucuski, MPT, administrator and physical therapist with the Magee-MossRehab at Voorhees (in New Jersey), as well as the entire staff, for their invaluable assistance with this article. Magee-MossRehab is an out-patient center that offers a comprehensive approach to evaluation and treatment for the individual with dysfunction due to the symptoms of MS.
Special thanks also go to Carrie Bruce, M.A., CCC-SLP, ATP, research scientist at the Center for Assistive Technology and Environmental Access (CATEA) at the Georgia Institute of Technology, Atlanta, Georgia. Accustomed to treating individuals with MS, her help with this article is greatly appreciated.
For More Information
National Rehabilitation Information Center
4200 Forbes Boulevard, Suite 202
Lanham, MD 20706
(800) 346-2742
(301) 459-5984 (TTY)
naricinfo@heitechservices.com
www.naric.com
National Clearinghouse of Rehabilitation Training Materials
1132 W. Hall of Fame
Oklahoma State University
Stillwater, OK 74078-4080
(800) 223-5219
(405) 744-2002 (TDD)
www.nchrtm.okstate.edu
American Physical Therapy Association
1111 North Fairfax Street
Alexandria, VA 22314-1488
(800) 999-APTA (2782)
(703) 683-6748 (TDD)
www.apta.org
American Occupational Therapy Association
4720 Montgomery Lane
PO Box 31220
Bethesda, MD 20824-1220
(301) 652-2682
(800) 377-8555 (TDD)
www.aota.org
American Speech-Language-Hearing Association
10801 Rockville Pike
Rockville, MD 20852
Toll-free, voice or TTY:
(800) 638-8255
www.asha.org
Magee Rehabilitation
Six Franklin Plaza
Philadelphia, PA 19102-1177
(800) 96-MAGEE (966-2433)
www.mageerehab.org
MossRehab Hospital
1200 West Tabor Road
Philadelphia, PA 19141-3099
(215) 456-9900
MossRehab
60 East Township Line Road
Elkins Park, PA 19027
(215) 663-6000
Other out-patient sites are listed in the web address:
www.mossresourcenet.org
(800) CALL MOSS (225-5667)
Georgia Tech Center for Assistive Technology and Environmental Access
490 Tenth Street, NW
Atlanta, GA 30332-0156
(800) 726-9119 (toll-free voice/TTY)
info@assistivetech.net
Shepherd Center
2020 Peachtree Road NW
Atlanta, GA 30309-1402
(404) 352-2020 (Main)
webmaster@shepherd.org
References
Burks JS, Johnson KP, Multiple Sclerosis; Diagnosis, Medical Management, and Rehabilitation, Demos Medical Publishing, New York, 2000.
Halper J, Holland N, Comprehensive Nursing Care in Multiple Sclerosis, second edition, Demos Medical Publishing, New York, 2002.
Schapiro R., Multiple Sclerosis, A Rehabilitation Approach to Management, Demos Medical Publishing, New York, 1999.
